Your burning COVID-19 questions, answered.
Living in the epicenter of the outbreak in the US has understandably raised a lot of concerns from my patients.
I’ve compiled the common questions I’ve heard and answered them to the best of my ability.
Some questions don’t have answers yet because we simply don’t have the data or research at this point (3/18/20).
I’ve linked sources wherever I can.
Please note: these answers are for informational purposes only. They are not medical advice. Please speak with your doctor or healthcare professional about what’s best for you.
I recommend checking out my other blog on how to keep yourself healthy as we wait this out.
Why is COVID-19 more potent than other coronaviruses?
This is a great question, and while I don’t have a direct answer, I do have some information that might help us to gain perspective.
Coronaviruses go around every year and tend to cause mild respiratory symptoms in the upper lungs.
They can result in an annoyingly persistent dry cough for a few weeks.
COVID-19, thought to originate from bats like SARS, is more potent because it has an affinity for the lower lung tissue, also like SARS*.
*SARS is a coronavirus.
The lower lungs are a more difficult place for your body to clear infection.
The lower lungs accumulate mucus, fluid, and inflammation more easily than the upper lungs and are common sites for pneumonia.
Air reaches them last and they are the deepest part of the tissue.
Why are certain people more vulnerable?
COVID-19, like SARS, binds to the angiotensin converting enzyme (ACE-2) receptor in our bodies.
ACE-2 receptors are found mostly in the lungs, intestine, kidney, and blood vessels and those tissues are being disproportionately affected by the virus.
Those with underlying conditions in these organs, like hypertension, cardiovascular disease, and diabetes are more vulnerable than others.
A class of drugs known as ACE inhibitors, commonly used to treat high blood pressure, upregulate ACE-2 receptors. Folks taking this medication could be more susceptible to COVID-19, as a higher number of viruses can bind in their lungs.
There aren’t studies that have proven this concept and most major medical societies are still recommending the use of ACE inhibitors currently, but looking at the co-morbidities of COVID-19 and mechanism of action of the virus, it’s a very plausible link.
If you want to get super nerdy, check out this detailed video.
Herbal BONUS tidbit: studies show that licorice was able to inhibit viral replication of SARS (another coronavirus). Licorice also makes it difficult for the virus to attach to its target cell, which is an ACE receptor.
Please note: this is not medical advice. I am not asking you to stop taking your blood pressure medication or to start taking licorice (which can raise your blood pressure). This is information to help you and your doctor make an informed decision based on your individual health needs.
Other populations more affected by COVID-19 are those over 65. Typically, we tend to have more health-related concerns as we age and our immune system has more to deal with.
The load on your system depends on a lot of factors and not everyone, even within a specific disease or age range, is going to be affected by COVID-19 identically. Read more about why that is here.
Disease processes like diabetes and heart disease point to a high load of chronic inflammation, largely in the blood vessels.
Chronic inflammation in any form -- from eating crappy, processed food, drinking alcohol, not enough sleep, from high blood sugar -- is a drain on your immune system.
Your immune cells are recruited to repair the damaged tissue that’s giving off the inflammatory signaling.
So the more inflammation you’ve got dancing around in your system at any one time, the more strain there is on your immune system to clean up the mess as well as protect and defend you from anything new coming in, like a virus.
Check out this video for a full list of conditions disproportionately affected by COVID-19, starting around 7 minutes (the whole video is full of great information).
How is it transmitted? Is it airborne?
To the best of the collective knowledge, COVID-19 is transmitted through droplets.
Droplets tend to have a range of about 3-6 feet.
So COVID-19 is technically airborne, but it is NOT aerosolized.
Aerosolization would carry the virus like a perfume and enable it to travel larger distances than 3-6 feet.
One study was able to aerosolize the virus into much smaller particles, but this was done artificially and there’s no evidence that it’s happening that way in nature.
What are the common symptoms?
Symptoms for COVID-19 are similar to cold, flu, and allergies, so it can be hard to distinguish early on.
The most common symptoms are fever, a dry cough, and shortness of breath.
COVID-19 tends to impact the lower airways and lungs, so there is often no sneezing or runny nose at the start. These symptoms are more common in upper respiratory illnesses like a cold.
Here’s an article on distinguishing your symptoms from a cold, allergies, or the flu.
And an infographic:
What should I do if I start to feel sick?
#1 Don’t panic.
#2 Self-quarantine even if you don’t feel that bad.
We’re still trying to reduce the spread of the virus. You might have mild symptoms (81% of COVID cases are mild), but the goal is to make sure people in more vulnerable groups like the elderly and those who have underlying conditions aren’t exposed.
#3 Call your doctor to discuss options.
Calling initially is better than going in because again, we want to reduce the spread of the virus.
COVID-19 tests are still few and far between in the US. Your state department of health is a good resource for finding the availability of COVID testing in your area.
Urgent care clinics are able to do general viral testing and may be able to help you identify a virus and rule out COVID-19.
Is COVID-19 susceptible to heat?
Studies from China published in February but still awaiting peer review do point to COVID-19 being susceptible to heat.
This new data also follows suit with previous coronaviruses.
Why is this important?
If the virus doesn’t survive well with heat it is likely that cases in the northern hemisphere will fall as the weather warms.
Cases in the southern hemisphere may increase as their weather cools.
Sunlight and being out in the fresh air may be helpful, if we look to our history, as UV light is helpful for killing viruses.
Humidity is another important factor.
The more humid the air, the more moisture it’s holding.
Droplets containing the virus get weighed down by the water more rapidly so they can’t stay airborne, causing them to fall to the ground.
It’s possible that there will be a resurgence of COVID-19 in the fall as temperatures cool.
The virus will have likely mutated by then, and hopefully into something less potent.
What kills COVID-19 on surfaces?
Fortunately regular cleaning products like 70% ethanol, hydrogen peroxide, and bleach can take care of COVID-19.
I would avoid the bleach if you can.
It’s a major respiratory irritant and could make you more susceptible to getting sick.
Let’s not give your body MORE stuff to deal with right now!
An interesting note is that copper surfaces naturally kill off tons of bugs, including superbugs and viruses.
We’ve seen that copper surfaces have killed coronaviruses before, so why aren’t hospitals using copper instead of stainless steel?
It’s a good question that will hopefully gain more traction within our medical system as the COVID-19 pandemic continues to develop.
Why the drastic precautions? I’m not in a high risk group.
To some, the local, state, and federal government recommendations to work from home, and limit activities and the size of social groups seems a bit much.
These folks have read up on the virus and who it impacts and have determined they’re in a low risk group and likely to have mild symptoms if they get sick.
It's important to realize that these recommendations aren't about you.
They’ve been put in place to protect the most vulnerable folks and our healthcare system.
Yes, 81% of cases are mild.
But 13% are severe and 4.8% are critical.
Severe and critical cases require hospitalization and resources like ventilators, and these resources are limited.
We’re seeing this healthcare system overload play out in Italy right now, with heartbreaking messages from exhausted doctors having to choose who gets treatment.
Comparing Italy to the US isn’t apples to apples.
Italy’s population is 60 million. The United States has a population of 327 million.
Italy has the largest percentage of people over 65 in Europe at 23%, increasing the potential for severe and critical cases.
Most deaths in Italy have been folks in their 80s and 90s and who are more susceptible to severe complications.
In good news, there have been at least 3 folks over 100 in China who survived COVID-19, living proof that age isn’t the only factor in the severity of illness.
By comparison, only 15.2% of the population in the United States is over 65.
But which country has more people with co-morbidities like hypertension, diabetes, and cardiovascular disease? I’d wager that the US does.
There are many variables at play that haven’t been sorted out or addressed yet.
That’s why it’s so hard to get accurate information.
The United States is doing an abysmal job testing for COVID-19.
Countries like South Korea that did extensive testing curbed the spread of the virus and reported a death rate of only 0.8%, as opposed to the 3.4% we’re seeing reported overall right now.
For comparison, the SARS epidemic in 2002 had a 15% mortality rate and H1N1 in 2009 had a mortality rate of 0.02%.
The COVID-19 mortality rate will most likely drop as we receive more data, as posited by this early-release research paper from Wuhan which estimates the mortality rate will be 0.25-3%.
As we scramble for accurate statistics without testing, this article transparently does the math for you.
He estimated that when the US had reported 22 deaths, there were actually 3,000 cases of COVID-19 in the country, not the 140 that had been reported at the time.
Another source I trust uses this formula: # of deaths x 200 = approximate # of cases.
So far, estimates put the spread rate at 2.2, meaning for every 1 sick person, 2.2 more are infected from that person. That’s double the R0 rate of the flu.
It’s estimated that 86% of cases in China were undocumented before the January 23rd travel shut down.
The bottom line is that COVID-19 is much more widespread than we think in the US.
I’m not saying that to scare you (again, 81% of cases are mild).
I’m saying that to put these government regulations in perspective.
There is just cause for caution.
Local resources in your area are incredibly important.
If an outbreak comes your way, will the city or small town you live in or around be able to get supplies and handle the capacity of people who need help?
Will there be enough hospital beds and masks?
This article estimates that at our current trajectory in the US we’ll be out of hospital beds by May 10th.
Obviously there’s a lot of best guesses happening, but it's definitely an interesting thought experiment to try to understand based on the current data what the impact on our healthcare system would be.
Even though videos and photos of families speaking to their elderly loved ones through windows or doors is heart wrenching, they’re doing the right thing.
For their loved ones and for the community.
What is social distancing?
This is a new term that seemed to conjure itself into existence a few days ago out of necessity to curb the spread of disease.
It’s about making smart choices about how you’re interacting with the world in an uncertain time.
Reducing your exposure to the virus can help you and it can really help others.
COVID-19 has a high and early viral shed rate, which means that people can pass on the virus well before they are symptomatic.
Researchers estimate the median incubation period at 5.1 days and they found that 97.5% of patients who have symptoms do so within 11.5 days of infection.
If you think you’ve been exposed to COVID-19, it’s advised that you self-quarantine for 14 days.
This is one reason why COVID-19 is spreading faster than a typical flu and governments are recommending more serious measures to contain it.
Older folks with underlying health conditions are being asked to stay home and younger people are being asked not to attend large events or go to bars or restaurants.
Check out this article for more answers to specific situations around social distancing.
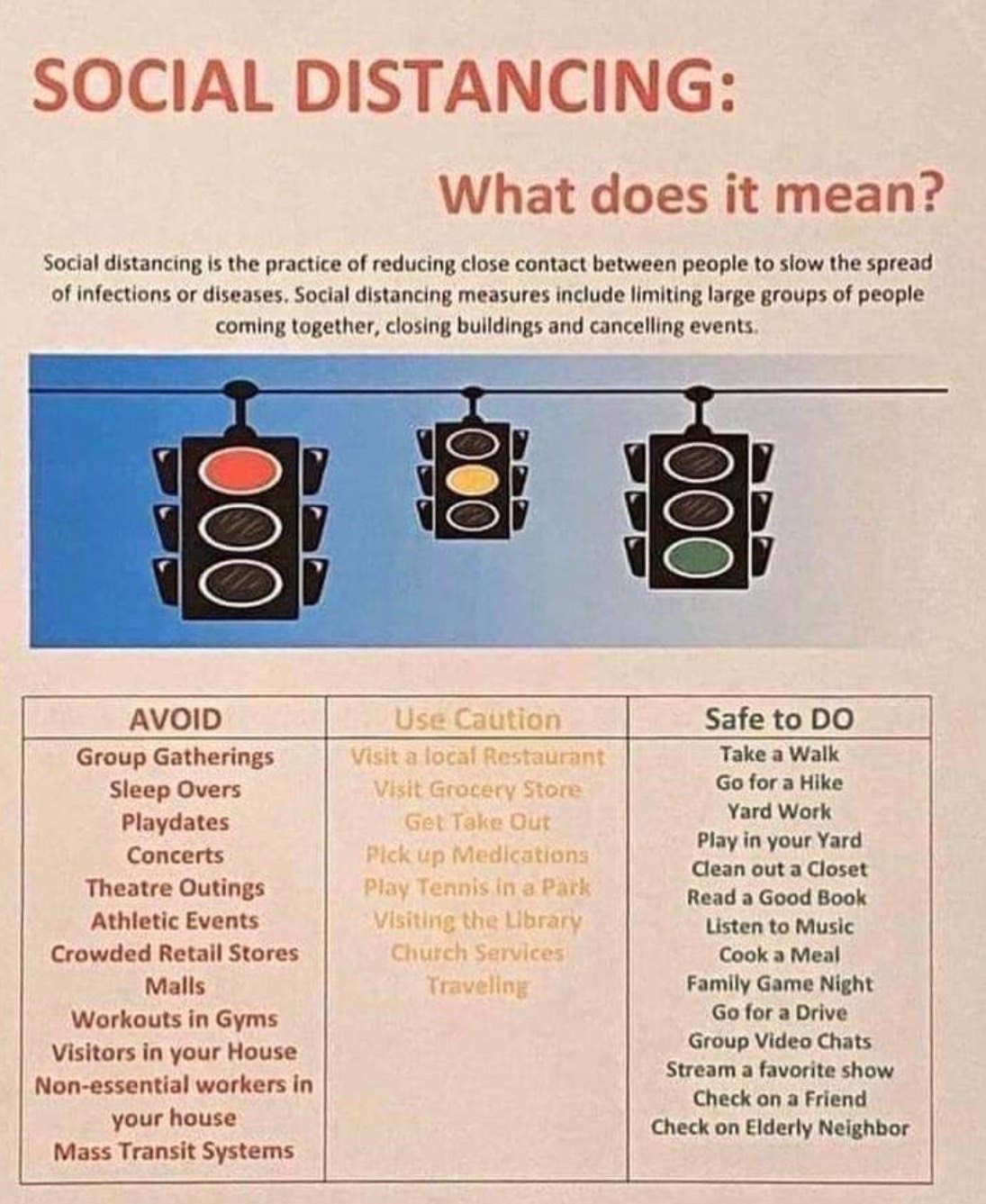
Here’s a handy infographic to help summarize recommendations:
As is the new mantra: wash your hands, don’t touch your face, try to keep a few feet of distance between you and others.
Should I wear a mask?
UPDATE 4/3/20: The CDC is now recommending wearing masks in public when social distancing measures are difficult to maintain to protect yourself and others.
For more information, please check out this article.
We know that the majority of transmission is happening through those who are infected by not yet sick or who are asymptomatic carriers of the virus.
Wearing a mask may help to reduce the spread of the virus.
However, there is still a massive shortage of personal protective equipment (PPE) for frontline healthcare workers.
Please consider making your own mask instead of buying one! There are tons of tutorials out there right now and all you need is 100% cotton fabric and a sewing machine.
You should not wear a mask unless you are actively sick, according to CDC guidelines.
The mask is more beneficial for containing droplets from the coughs or sneezes of sick patients than it is for preventing the infection of healthy people.
A mask shortage is affecting frontline healthcare workers interacting with sick patients.
Please stop buying masks so healthcare workers can remain safe and adequately protected.
Should I expose myself purposefully to COVID-19 to get antibodies?
Please DO NOT DO THIS.
For several reasons.
#1 Social distancting is there for a reason
As mentioned above, we are trying to DECREASE THE SPREAD of the virus right now so as not to overwhelm the healthcare system.
#2 Antibodies don't stick around
A survey of SARS patients (another coronavirus) 5 and 10 years after their recovery showed a low level of antibodies to the virus.
You might develop short term immunity, but that really doesn’t help you in the long run if you’re exposed to another coronavirus in the future.
#3 Seasonal viruses rapidly mutate
Coronaviruses, influenza, and other seasonal viruses mutate quickly.
If you catch COVID-19 now, you’ll likely have partial to no immunity to the next iteration that goes around in the fall or the next year.
It’s similar to good ol’ influenza. Rapid genetic changes in the virus allow it to sneak past our immune system.
This is exactly why the accuracy of the flu vaccine is so up and down year by year.
Scientists literally have to guess which strain might pop up and hope they get it right.
#4 COVID-19 is NOT like chickenpox
I have heard comments about getting together for COVID-19 parties like chickenpox parties just to “get it over with” and develop antibodies.
Chickenpox, or varicella zoster, is NOT a rapidly mutating virus.
If you are exposed a second time, the antibodies from your first infection will most likely fend off a new exposure handily because the virus has not really changed that much and is still recognized by your immune system.
Another layer to the chickenpox comparison is that since it’s in the herpes virus family, once you have it, it stays with you for life.
The virus lives in one particular grouping of nerves and that group varies from person to person.
A healthy immune system can keep the virus in check. Antibodies are constantly there to keep it from replicating.
The COVID-19 virus, like the flu virus, does not stay in your system.
What about vaccines? Are they our best bet?
If anyone reading this article watches Letterkenny: Hard no.
A mentor of mine, Dr. Nancy Welliver, summed up issues with vaccination beautifully:
“Because of the ability of viruses to quickly and continuously adapt, the odds of us meeting, as a species, novel viruses is infinitely high. This is why relying on immunizations is folly, and providing good lifestyle based medicine is the best course. Right now, the estimate for the arrival of an immunization is 9-12 months. By then the virus will have hit the susceptible hosts, and will probably have mutated, making the immunization fairly ineffective, as we have seen with successive years of flu immunization. Promoting a healthy immune system is the best defense.”
Even if the estimated timeline for a vaccine speeds up, we will likely be dealing with a mutated strain.
Read my previous article on how to promote a healthy immune system.
You can be proactive and protect yourself!
I heard elderberry isn’t safe. What’s the deal?
Please do not be afraid of taking elderberry.
It’s a truly wonderful antiviral herb that’s been used for centuries to treat seasonal flus and viruses.
It works by ”inhibiting the early stages of an infection by blocking key viral proteins responsible for both the viral attachment and entry into the host cells," one study concluded.
Unfortunately it’s pretty much sold out everywhere right now, but file that tidbit away for when it comes back into stock and you’re wanting a great preventative and acute herb on hand!
Elderberry and another commonly used immune herb, Echinacea, came under fire because of a phenomenon that’s been happening in late stage COVID-19 cases called a cytokine storm.
Let’s break this down.
Cytokines are part of the inflammatory cascade, or the signaling process that tells your body there’s an invader present or something is amiss and it needs to be checked out by the immune system.
A cytokine storm happens when a TON of these signaling proteins get released at once.
Essentially, the immune system goes bonkers trying to fight the virus and can end up damaging the organs and tissues of the host.
A common cytokine is interleukin-6 or IL-6, and studies have shown that elderberry can increase IL-6.
Yes, elderberry can increase IL-6, but not to the level of a cytokine storm.
That is fundamentally not how elderberry, most immune herbs, or herbs in general, work.
The real beauty of herbs like elderberry and echinacea is that they help your immune system adapt to whatever is going on.
In other words, they aren’t drugs.
They’re not going to overstimulate your body, they’re going to work with it.
And they certainly aren’t going to create or exacerbate a cytokine storm.
Polyphenols, triterpenoids, and flavonoids, all from herbs, may potentially be active components in protecting AGAINST a cytokine storm during severe influenza, one study found.
Echinacea has been shown to decrease cytokines in immune responses.
We must take the WHOLE plant and WHOLE cytokine response into mind.
It is impossible to separate out each component, look at reactions, and think we have an accurate understanding of a complex, interrelated, integrated system.
What’s interesting about a cytokine storm (yes, I did just say that) is that it’s not all about inflammation, even though that’s typically what everyone focuses on.
There are non-inflammatory portions of the cytokine storm that facilitate viral clearance and promote tissue repair, and regulate the severity of the inflammatory cytokines.
Here’s an excerpt from well known herbalist, Paul Bergner:
…[H]erbalists cannot take an isolated experiment showing the effect of an herb or its constituents on a single cytokine, and extrapolate that to the net effect of the plant on the whole spectrum of cytokines. In fact both Echinacea and Sambucus have been shown to stimulate immunoregulatory cytokines, with a net non-inflammatory effect. Elderberry extracts were shown to enhance both inflammatory and anti-inflammatory cytokines in human cells in lab experiments (Barak et al.). In another lab study, an extract of Sambucus flowers inhibited all pro-inflammatory cytokines measured (Harokopakis et al.) Another yet another showed regulation through partial inhibition of inflammatory cytokines (Yesilada et al). One trial of the use of a combination of Echinacea and Eupatorium perfoliatum found no net inflammatory effect produced by cytokines in humans at the dose tested (Elsasser-Beile et al.) Researchers at University of British Columbia who have studied Echinacea extensively concluded that the plant has a net anti-inflammatory effect, while maintaining “direct and selective” antiviral and antibacterial activity. In infected cell media, genes that code for proinflammatory cytokines, were stimulated by the pathogens, but Echinacea reversed the effects. A study showed that infection with virus or bacteria in cell arrays induced secretion of pro-inflammatory cytokines, but that this was also reversed by Echinacea (Hudson et al). (source)
The cytokine storms happened in late stage COVID-19 patients.
It is not brought on by herbs, but as a last ditch effort by the body to right the ship.
What can we do to help keep our immune system strong?
Do:
Hop on over to my other post all about how to stay healthy.
There are tons of great ideas! There’s so much more that you can do for your health than wash your hands, don’t touch your face, and socially isolate.
I see these things make huge differences in my patients’ lives every day, whether they are dealing with chronic illness, or something acute like a flu or cold.
Don’t:
Have any non-emergency or elective procedures or surgeries done for the next 2-4 weeks, especially if you are over 60.
Your immune system doesn’t need more stress at this moment in time.
Let it defend you to its fullest potential rather than asking it to multi-task and leave you more susceptible.
Wait until things start to settle and there are less cases.
Don’t:
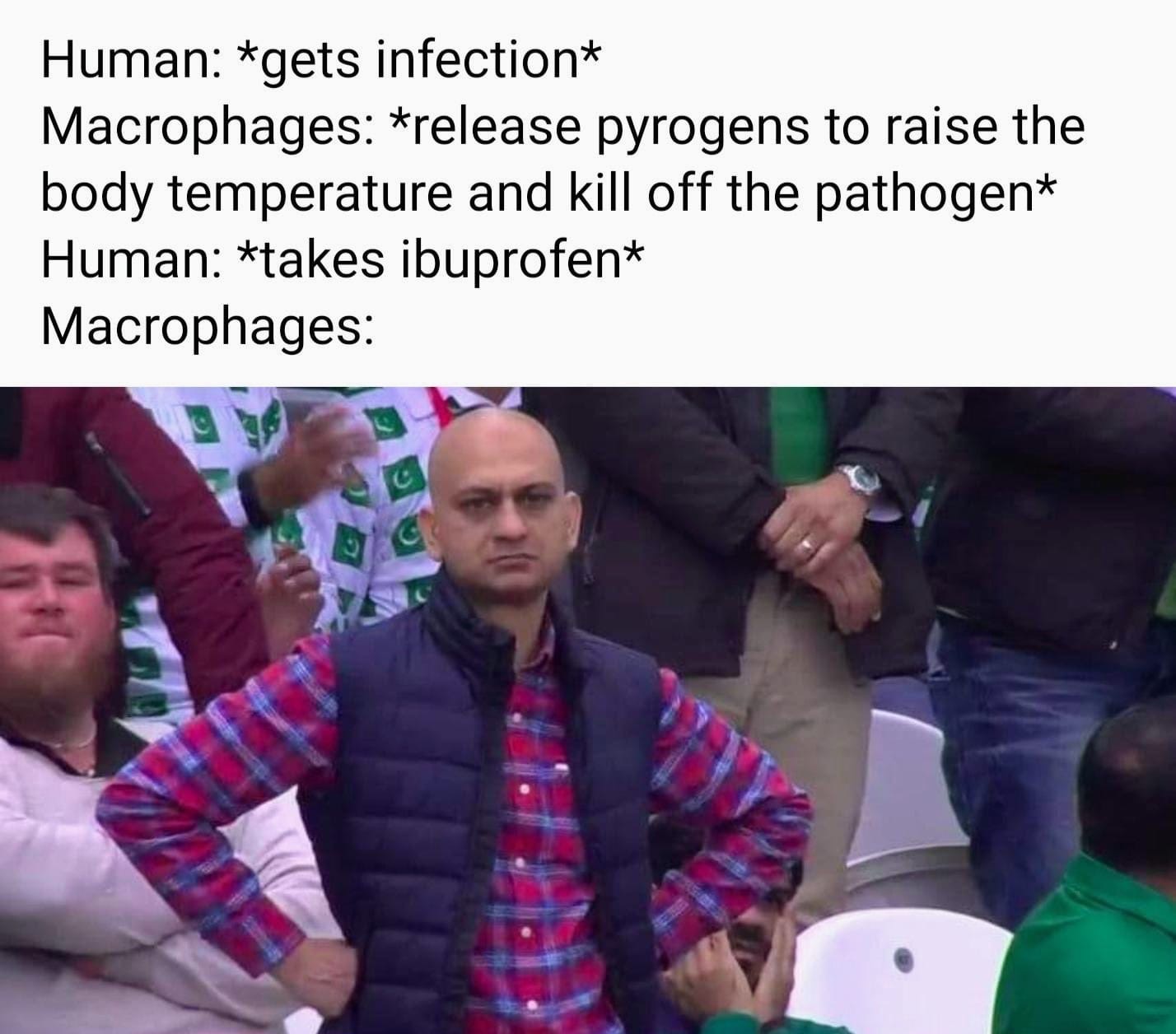
Take fever reducers.
Especially don’t take them if you are sick with a cold, flu, or potentially COVID-19.
Of course they do!
Your body is creating a fever to kill the virus off, as it can’t live at higher temperatures. Fevers also help to recruit immune cells.
By taking a fever reducer you’re asking your body to fight the infection AND the drug at the same time.
Clinically I have seen people double their acutely sick time when they take fever reducers.
Here’s a great visual for you:
I disagree.
Skip them both.
Focus on rest, hydration, easy to digest food, and let your body do its work. Don’t get in the way.
For all of you detailed, science-oriented folks, here’s a great overview of the current information we have.
I hope this helps answer some of your questions.
Stay safe, don’t panic, and keep your immune system strong.